Understanding the Overlap Between Dysautonomia & Multiple Sclerosis
Explore the POTS and MS connection, how dysautonomia overlaps with multiple sclerosis, and what it means for diagnosis, symptoms, and treatment strategies.
Postural Orthostatic Tachycardia Syndrome (POTS) and Multiple Sclerosis (MS) are both complex neurological conditions. When they appear together, the relationship can cause confusion for patients and challenges for healthcare providers. This post explores the POTS and MS connection, uncovering how dysautonomia often overlaps with multiple sclerosis and what that means for diagnosis, symptoms, and treatment.
Recap | What Is POTS?
Postural Orthostatic Tachycardia Syndrome (POTS) is a form of dysautonomia, meaning it affects the autonomic nervous system, which controls involuntary bodily functions like heart rate, digestion, and blood pressure regulation. POTS primarily disrupts circulation and vascular tone, leading to difficulty maintaining blood flow when changing positions—particularly when standing.
What is the biggest dietary challenge you face with POTS?

Key Symptoms of POTS
Temperature regulation issues
Dizziness and lightheadedness upon standing
Rapid heartbeat (tachycardia) triggered by postural changes
Chronic fatigue due to circulatory instability
Brain fog and difficulty concentrating
Why POTS Is Often Misunderstood
Since POTS does not always present with visible symptoms, individuals may struggle to explain their condition or receive proper diagnosis. It can significantly impact daily activities, leading to exercise intolerance, difficulty standing for extended periods, and unpredictable energy fluctuations.
What Is Multiple Sclerosis?
Multiple Sclerosis or just MS is a chronic autoimmune disease in which the immune system mistakenly attacks the protective myelin sheath surrounding nerves in the central nervous system. This leads to neurological dysfunction, causing disruptions in muscle control, sensory processing, and cognitive function.
Common Symptoms of MS
Cognitive and memory issues
Muscle weakness and spasticity
Vision disturbances (blurry vision, optic neuritis)
Difficulty with balance and coordination
Nerve pain and tingling sensations
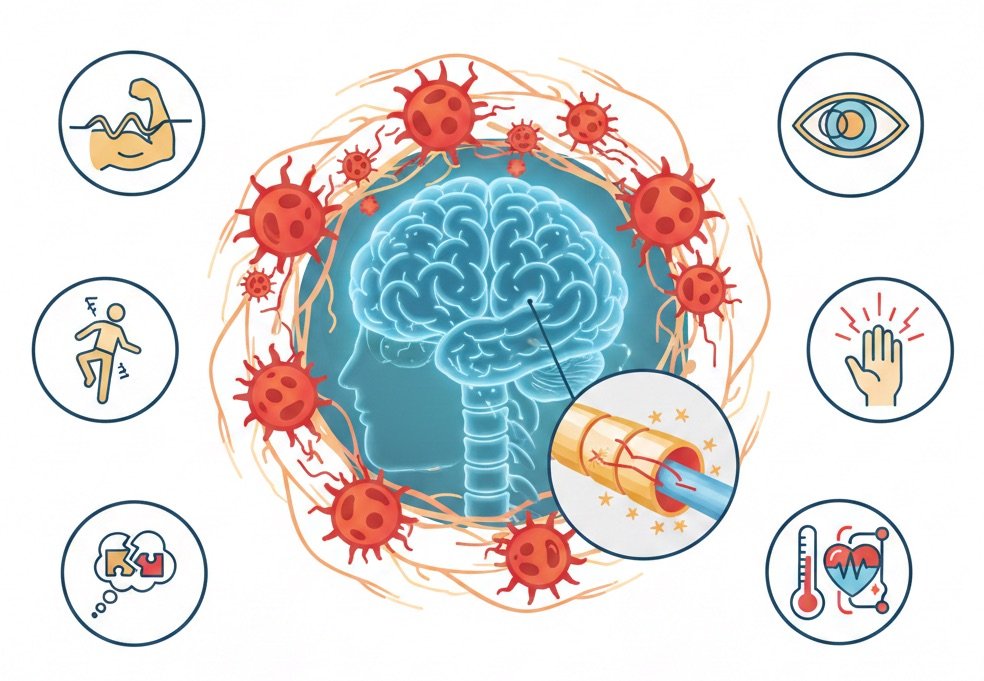
Autonomic Dysfunction in MS
While MS is primarily recognized for its neurological impairments, many individuals also experience dysautonomia-related symptoms, including irregular blood pressure, circulation issues, and temperature sensitivity. This is where the connection between MS and POTS begins, as both conditions share autonomic instability that disrupts normal vascular and heart rate regulation.
How the POTS and MS Connection Happens
The link between POTS and MS stems from autonomic nervous system dysfunction, which plays a crucial role in regulating heart rate, blood pressure, circulation, and temperature control.
Impact of MS Lesions on Autonomic Function
MS is characterized by demyelination, where the immune system attacks the protective myelin sheath surrounding nerve fibers in the central nervous system (CNS). When these lesions occur in areas like the brainstem, spinal cord, or autonomic control centers, the body struggles to regulate involuntary processes, leading to symptoms that resemble POTS.
Secondary POTS in MS Patients
Some individuals with MS develop secondary POTS as a result of damage to autonomic pathways within the central nervous system (CNS). This disrupts blood pressure stability and heart rate regulation, making orthostatic intolerance more pronounced.

Independent Coexistence of POTS and MS
In some cases, POTS and MS occur separately but with overlapping symptoms that intensify daily challenges. Determining whether POTS is a secondary condition linked to MS or an independent diagnosis is essential for developing targeted treatment strategies.
Symptoms That Overlap Between POTS and MS
Since both conditions impact nervous system function, many symptoms overlap, making diagnosis and differentiation difficult.
Common Symptoms Present in Both POTS and MS
- Dizziness and lightheadedness – Especially upon standing due to circulation instability
- Chronic fatigue – A hallmark of both conditions linked to autonomic dysfunction
- Brain fog and cognitive difficulties – Impaired focus and memory challenges
- Heat intolerance – Difficulty regulating body temperature in warm environments
- Bladder and bowel dysfunction – Disruptions in autonomic control over digestion and urinary function
- Muscle weakness – Neurological impairment in MS, circulatory strain in POTS
- Palpitations – Heart rate irregularities commonly seen in dysautonomia
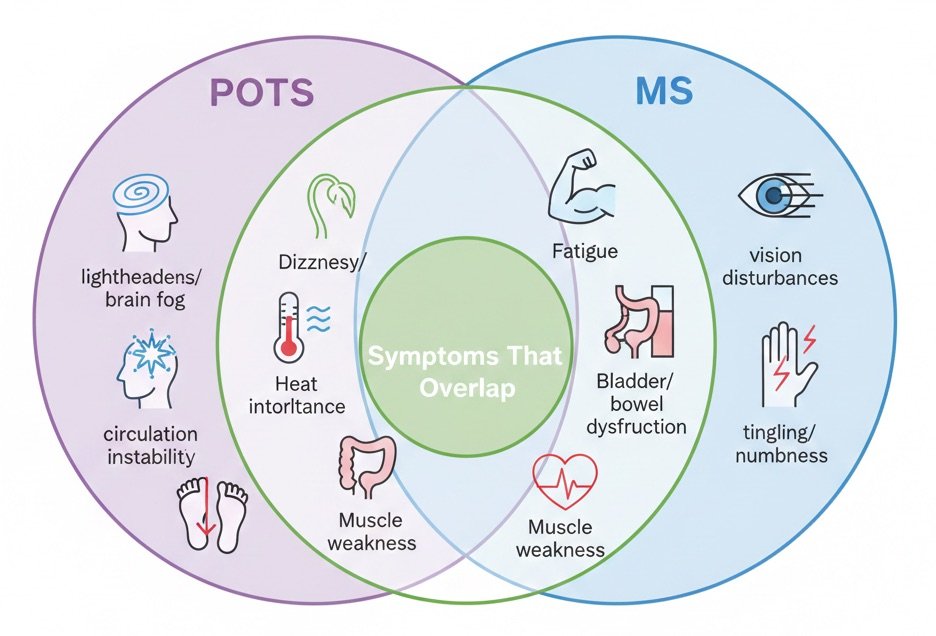
Importance of Recognizing Overlapping Symptoms
Since many of these symptoms can result from either autonomic dysfunction or demyelination, correctly identifying their root causes is essential for effective symptom management. Comprehensive evaluations, autonomic function tests, and neurological assessments are key to differentiating POTS from MS-related dysautonomia.
Diagnosing the POTS and MS Connection
Proper diagnosis begins with recognizing the distinct and overlapping symptoms of both POTS and MS. Since POTS affects autonomic regulation, and MS disrupts central nervous system function, diagnostic clarity is essential to determine whether POTS is secondary to MS or an independent condition.
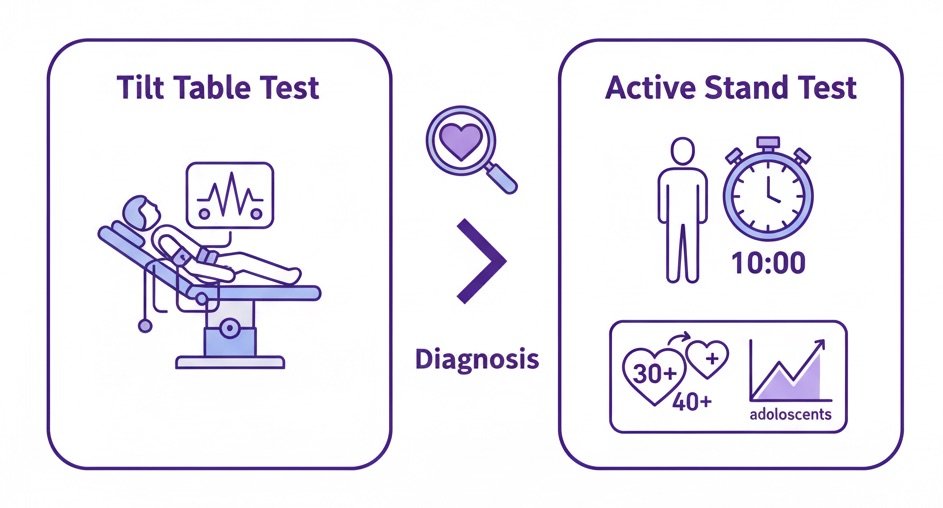
Key Diagnostic Methods for POTS
Because POTS involves heart rate irregularities upon standing, specialized autonomic testing is necessary to confirm its presence.
Active Stand Test – Assesses whether heart rate increases by 30+ bpm in adults or 40+ bpm in adolescents within 10 minutes of standing
Tilt Table Test – Measures heart rate and blood pressure fluctuations when transitioning from a lying to standing position
Key Diagnostic Methods for MS
MS is primarily diagnosed using neurological imaging and cerebrospinal fluid analysis, which help detect demyelination and immune system activity within the central nervous system.
- MRI Scans – Identify lesions on the brain and spinal cord, a hallmark of MS
- Lumbar Puncture (Spinal Tap) – Detects abnormal immune markers in cerebrospinal fluid
Investigating POTS-Like Symptoms in MS Patients
If a patient already diagnosed with MS experiences symptoms resembling POTS, specialists may need to assess autonomic nervous system function more thoroughly.
- Comprehensive Autonomic Testing – Includes heart rate variability, blood pressure monitoring, and thermoregulatory sweat tests
- Neurological Workup – Determines whether autonomic instability is caused by MS-related lesions or separate dysautonomia
Why Proper Differentiation Matters
Since POTS and MS share common symptoms, misdiagnosis or incomplete evaluations can delay appropriate treatment strategies. Understanding whether POTS is secondary to MS or a coincidental diagnosis enables targeted symptom management, improving daily functionality and overall well-being.
Treating POTS in Patients With MS
Managing POTS in patients with MS requires a careful, multi-faceted approach, addressing both autonomic dysfunction and nervous system damage simultaneously. Since MS can directly impact autonomic regulation, treatment must balance cardiovascular support with neuroprotective strategies.
Lifestyle Modifications
Simple lifestyle changes can help reduce symptoms of orthostatic intolerance and support circulation.
- Increase fluid and salt intake – Helps maintain blood pressure and blood volume
- Wear compression garments – Reduces blood pooling in the legs, minimizing dizziness
- Elevate the head of the bed – Supports blood flow regulation during sleep
Exercise Programs
While exercise must be carefully tailored to avoid exacerbating symptoms, it plays a crucial role in strengthening cardiovascular health and autonomic stability.
- Gentle, recumbent exercises (cycling, swimming) – Build fitness while minimizing orthostatic stress
- Strength training for lower body circulation – Helps improve vascular tone and blood pressure regulation

Medications
Medications may be required to support blood pressure, heart rate stabilization, and autonomic function.
- Beta blockers – Help control tachycardia and excessive heart rate fluctuations
- Fludrocortisone – Aids blood volume retention, supporting hydration levels
- Midodrine – Increases vascular tone, reducing blood pressure instability

MS-Specific Therapies
Since MS-related lesions can worsen autonomic symptoms, treating MS progression is equally vital.
- Disease-modifying therapies – Aim to slow further nerve damage and inflammation
- Neurological rehabilitation programs – Help improve motor function and balance
Personalized Treatment Approach
Every patient’s condition is unique, and treatment plans must be individually customized to address the interaction between MS and dysautonomia-related symptoms.

Living With Both POTS and MS
Navigating life with both MS and POTS requires a holistic approach, ensuring symptom control, emotional resilience, and daily functionality.
Working with a Multidisciplinary Team
Patients benefit from a collaborative medical approach, involving:
- Neurologists to monitor MS progression
- Cardiologists to regulate heart rate and blood pressure
- Physical therapists for mobility and circulation support
Key Strategies for Daily Management
- Energy conservation techniques – Helps avoid excess fatigue and symptom flare-ups
- Symptom tracking – Identifies triggers, guiding treatment adjustments
- Mental health support – Counseling and mindfulness practices improve coping and stress management
Patient Advocacy and Empowerment
Understanding the POTS and MS connection empowers individuals to seek specialized care, advocate for personalized treatment, and adopt strategies that enhance long-term quality of life.

GnarlyTree | EXERCISE GUIDE
Best Exercise Equipment for POTS | Tools for Safe & Effective Workouts
Why Exercise is Important for POTS Management Finding the Best Exercise Equipment for POTS is important. Managing Postural Orthostatic Tachycardia Syndrome requires a strategic approach to exercise, incorporating tools that promote circulatory stability, heart rate...
Frequently Asked Questions
How are POTS and MS connected?
Both conditions involve autonomic dysfunction, but in MS, demyelination in the central nervous system can interfere with the regulation of heart rate and blood pressure, sometimes leading to POTS-like symptoms.
Can MS cause secondary POTS?
Yes, MS lesions affecting autonomic control centers can lead to secondary POTS, where autonomic dysfunction arises due to nerve damage rather than an independent condition.
What symptoms overlap between POTS and MS?
Both conditions can cause dizziness, fatigue, brain fog, heat intolerance, bladder issues, muscle weakness, and palpitations, making diagnosis more complex.
How is POTS diagnosed in MS patients?
Doctors may use a Tilt Table Test or Active Stand Test to observe heart rate increases upon standing, alongside MRI scans and lumbar punctures to confirm MS-related autonomic dysfunction.
What lifestyle changes help manage both conditions?
Increasing fluid and salt intake, wearing compression garments, and engaging in low-impact exercises can improve circulation and symptom stability.
Can medications help with POTS symptoms in MS patients?
Yes, medications such as beta blockers, fludrocortisone, and midodrine can regulate heart rate, blood pressure, and vascular tone, but must be tailored to individual needs.
How does physical therapy help with both MS and POTS?
A structured physical therapy program helps strengthen connective tissues, improve circulation, and enhance postural stability, reducing dizziness and muscle weakness.
Are disease-modifying treatments for MS necessary when managing POTS?
Yes, slowing MS progression with disease-modifying therapies is essential, as continued nerve damage can worsen autonomic dysfunction and impact POTS symptoms.
Why is patient advocacy important for those with both conditions?
Advocating for comprehensive autonomic testing and multidisciplinary care ensures that individuals receive targeted treatments for both MS and POTS-related symptoms.
Conclusion
The link between Postural Orthostatic Tachycardia Syndrome (POTS) and Multiple Sclerosis (MS) underscores the intricate relationship between neurological disorders and autonomic dysfunction. Recognizing how these conditions intersect allows for more effective diagnosis, treatment, and symptom management, ensuring that patients receive specialized care tailored to their unique needs.
As research continues to advance, greater awareness and medical innovation will pave the way for improved outcomes and enhanced quality of life for individuals managing both POTS and MS. By fostering a deeper understanding of autonomic regulation in neuroimmune diseases, healthcare professionals can refine treatment strategies and empower patients with knowledge-driven solutions for long-term care.
Do you use an adjustable bed or special pillows for sleep?