Understanding the Tilt Table Test for POTS
The Tilt Table Test is a crucial diagnostic procedure commonly used to identify Postural Orthostatic Tachycardia Syndrome (POTS), a form of dysautonomia. Patients experiencing unexplained dizziness, rapid heart rate upon standing, lightheadedness, or fainting episodes often undergo this test to determine the underlying cause of their symptoms. In this comprehensive guide, we will explore how the Tilt Table Test works, its role in diagnosing POTS, what patients can expect during the procedure, and how to interpret the results.
What is a Tilt Table Test?
A Tilt Table Test is a non-invasive method used to evaluate how the body responds to changes in posture, particularly from lying down to standing up. It monitors cardiovascular responses, including heart rate and blood pressure, which are essential for identifying conditions like POTS, neurally mediated hypotension, and orthostatic hypotension.
During the test, a patient is secured to a motorized table that tilts them from a horizontal to a vertical position while vital signs are continuously recorded. The objective is to simulate the body’s response to standing without requiring the patient to actively change positions.
What is the biggest dietary challenge you face with POTS?
Why is the Tilt Table Test Used for POTS?
POTS is characterized by an exaggerated increase in heart rate—typically a jump of 30 beats per minute or more (or over 120 bpm total) within 10 minutes of standing, without a significant drop in blood pressure. The Tilt Table Test creates a controlled environment to observe this autonomic nervous system dysfunction.
Key reasons for using the Tilt Table Test in POTS diagnosis include:
- Assessing orthostatic intolerance
- Distinguishing POTS from other forms of dysautonomia
- Identifying abnormal autonomic nervous system responses
- Confirming suspected POTS when clinical symptoms align
How the Test is Performed
The procedure generally takes 30 to 60 minutes and is performed in a hospital or specialized autonomic testing clinic.
Preparation
- Patients are advised to fast for at least 4-6 hours before the test.
- Caffeine, alcohol, and certain medications may need to be avoided prior to testing.
- Comfortable clothing is recommended.
Step-by-Step Process
- Baseline Monitoring: The patient lies flat on the tilt table, and baseline heart rate and blood pressure are recorded.
- Tilting Phase: The table is tilted to an angle, usually between 60 and 80 degrees, simulating standing upright.
- Observation Period: The patient remains tilted for up to 45 minutes while monitoring continues.
- Return to Supine: If symptoms develop or sufficient data is collected, the patient is returned to the flat position.
Optional Provocation
Some tests include medication such as isoproterenol or nitroglycerin to provoke a stronger response if initial results are inconclusive.
What to Expect During and After the Test
Possible Sensations
- Lightheadedness or dizziness
- Palpitations or rapid heartbeat
- Nausea or sweating
- Fatigue
These symptoms help clinicians identify autonomic dysfunction but are closely monitored to ensure patient safety.
Aftercare
Most patients can resume normal activities shortly after the test, though some may feel fatigued for the rest of the day. Drinking fluids and resting are recommended post-procedure.
Interpreting the Results
Positive Result for POTS
- Heart rate increases by 30+ beats per minute within 10 minutes of tilting (or over 120 bpm total)
- No significant drop in blood pressure
- Symptoms such as dizziness or palpitations are reported
Other Possible Diagnoses
- Orthostatic Hypotension: A significant drop in blood pressure when tilted
- Neurally Mediated Hypotension: Sudden drop in both heart rate and blood pressure
- Normal Response: Mild, brief increases in heart rate and blood pressure without symptoms
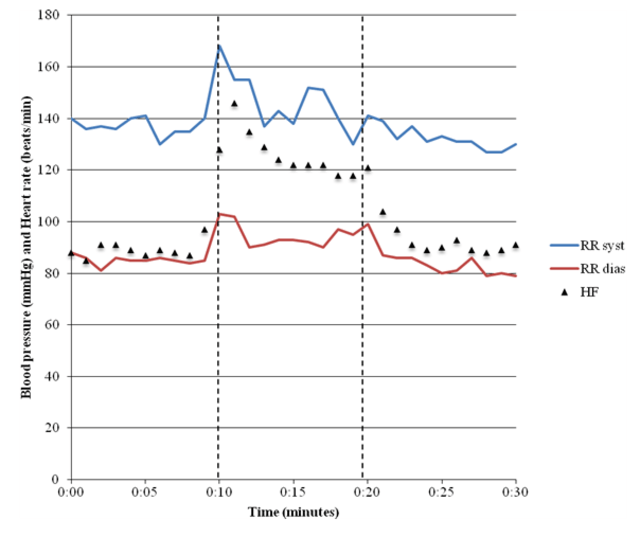
Legend:
Diastolic blood pressure (RED)
Systolic blood pressure (BLUE)
Heart rate (BLACK)
Limitations of the Tilt Table Test
While invaluable, the Tilt Table Test has some limitations:
- Not 100% definitive—false positives and negatives can occur
- May not replicate real-life symptom triggers
- Results can vary depending on hydration, anxiety, or medication use
Still, it remains a cornerstone in diagnosing POTS and other forms of dysautonomia when combined with clinical evaluation and patient history.
Complementary Tests and Follow-Up
After a positive Tilt Table Test, additional diagnostic tools may include:
- 24-hour Holter monitoring
- Autonomic reflex screening
- Blood volume studies
- Catecholamine testing
A multidisciplinary approach including cardiology, neurology, and primary care is often recommended for comprehensive management.
Lifestyle and Treatment Implications Post-Diagnosis
A confirmed POTS diagnosis through a Tilt Table Test can lead to targeted treatments:
- Increased fluid and salt intake
- Use of compression garments
- Regular recumbent exercise
- Medications like beta blockers, fludrocortisone, or midodrine
Lifestyle changes are often just as important as pharmacological interventions in managing symptoms.

GnarlyTree | COMPLEMENTARY THERAPIES
Can Acupressure Help with POTS? | Exploring Alt Treatment Options
Can Acupressure Help with POTS? As patients search for complementary strategies beyond pharmaceutical interventions, acupressure—a technique rooted in Traditional Chinese Medicine (TCM)—is gaining attention as a gentle, non-invasive way to regulate nervous system imbalances. This...
🩺 FAQ: Tilt Table Test and POTS
1. What is a Tilt Table Test?
It’s a non-invasive procedure that evaluates how your heart rate and blood pressure respond to changes in posture, particularly moving from lying to standing.
2. Why is the Tilt Table Test used to diagnose POTS?
It helps identify the hallmark POTS response—an exaggerated heart rate increase upon standing—while ruling out other causes of orthostatic symptoms.
3. How is the Tilt Table Test performed?
You’re secured on a motorized table, tilted upright while your vitals are monitored, and observed for up to 45 minutes for abnormal responses.
4. What symptoms might occur during the test?
You may feel dizzy, lightheaded, nauseous, or experience a racing heart—these symptoms help confirm autonomic dysfunction.
5. How should I prepare for the test?
Avoid food, caffeine, alcohol, and certain medications for several hours beforehand; wear comfortable clothing.
6. What does a positive test for POTS look like?
A heart rate increase of 30+ bpm within 10 minutes of tilting (or exceeding 120 bpm) without a major drop in blood pressure.
7. Are there limitations to the Tilt Table Test?
Yes, results can vary and false positives or negatives are possible; it may not always reflect real-life symptom triggers.
8. What happens after the test?
Most people can resume normal activities, though some feel tired—hydration and rest are usually advised.
9. What other conditions can the test detect?
It can also diagnose orthostatic hypotension and neurally mediated hypotension based on different heart rate and blood pressure responses.
10. What comes next if I’m diagnosed with POTS?
Treatment may include increased fluids and salt, compression wear, exercise, medications, and lifestyle changes tailored to your symptoms.
Conclusion
The Tilt Table Test is a pivotal tool in diagnosing POTS, offering a controlled method to evaluate how the autonomic nervous system responds to changes in posture. While it is not without its limitations, its role in identifying POTS and related disorders is indispensable.
If you are experiencing symptoms like dizziness, rapid heartbeat upon standing, or chronic fatigue, consult with your healthcare provider to determine if a Tilt Table Test is appropriate. Early diagnosis can lead to better management and improved quality of life.
Do you use cold packs or heat pads to manage symptoms?



