For many people, POTS is only one part of a much larger health picture. When symptoms overlap, fluctuate, or appear suddenly, it becomes difficult to know what is caused by POTS, what stems from another condition, and what might be related to lifestyle factors such as nutrition, hydration, stress, sleep, or exercise routines.
This guide explores how to sort through symptoms, recognize patterns, and understand the complex interplay between POTS and coexisting conditions. It is designed for people who live with multiple diagnoses and want clarity—not medical advice—on how to interpret what their bodies are telling them.
Why It’s Hard to Know What Symptoms Come From POTS
POTS affects the autonomic nervous system, which regulates heart rate, blood pressure, digestion, temperature, and circulation. Because the autonomic system touches nearly every part of the body, POTS symptoms can appear almost anywhere.
Which diagnostic test was most helpful for your diagnosis?
Common POTS symptoms include:
- Lightheadedness and dizziness
- Rapid heart rate when standing
- Fatigue and exercise intolerance
- Brain fog and cognitive difficulty
- Temperature dysregulation
- Nausea or digestive discomfort
- Muscle weakness or shakiness
But when you also live with conditions like Ehlers‑Danlos syndrome (EDS), mast cell activation issues, migraines, autoimmune disorders, chronic pain conditions, neuropathy, or nutritional deficiencies, the symptom list becomes a tangled web.
This is why so many people ask:
“Is this POTS… or something else?”

Understanding Symptom Overlap in POTS and Coexisting Conditions
When Multiple Conditions Share the Same Symptoms
Many chronic conditions share overlapping symptoms with POTS, including:
- Fatigue
- Pain
- Dizziness
- GI issues
- Cognitive changes
- Temperature sensitivity
- Sleep disturbances
This overlap makes it difficult to pinpoint the source of a new or worsening symptom. For example:
- Bone or joint pain may be related to hypermobility, inflammation, nutritional deficiencies, or neuropathy—not necessarily POTS.
- Severe fatigue may come from POTS, anemia, thyroid issues, sleep disorders, or medication side effects.
- Heart palpitations may be POTS, dehydration, anxiety, or unrelated cardiac issues.
Understanding the pattern of symptoms is often more helpful than trying to assign each symptom to a single cause.

How to Tell When a Symptom Is Likely From POTS
While POTS symptoms vary widely, certain patterns tend to point toward autonomic dysfunction.
Symptoms That Often Worsen With Position Changes
If symptoms intensify when you:
- Stand up
- Walk for long periods
- Shower
- Get overheated
- Are dehydrated
…they may be more related to POTS.
Symptoms That Improve With Rest or Recumbent Positions
If lying down, elevating your legs, cooling off, or hydrating helps, the autonomic system is likely involved.
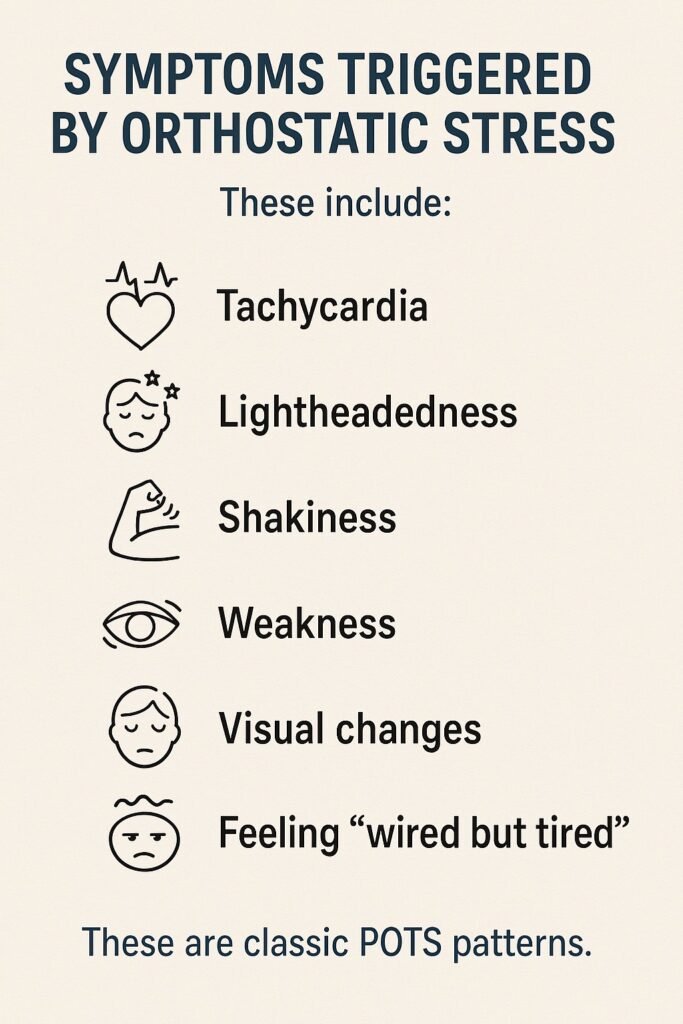
Symptoms Triggered by Orthostatic Stress
These include:
- Tachycardia
- Lightheadedness
- Shakiness
- Weakness
- Visual changes
- Feeling “wired but tired”
These are classic POTS patterns.

When Symptoms Are More Likely From Other Conditions
Pain That Doesn’t Change With Position
Bone pain, deep joint pain, or localized inflammation often points to:
- Hypermobility or EDS
- Arthritis
- Nutrient deficiencies
- Neuropathy
- Autoimmune activity
- Overuse or injury
POTS itself does not typically cause bone pain.
Symptoms That Follow Food, Allergens, or Environment
If symptoms flare after eating, exposure to scents, or environmental triggers, they may relate to:
- Mast cell activation
- Food sensitivities
- Histamine intolerance
- Blood sugar fluctuations
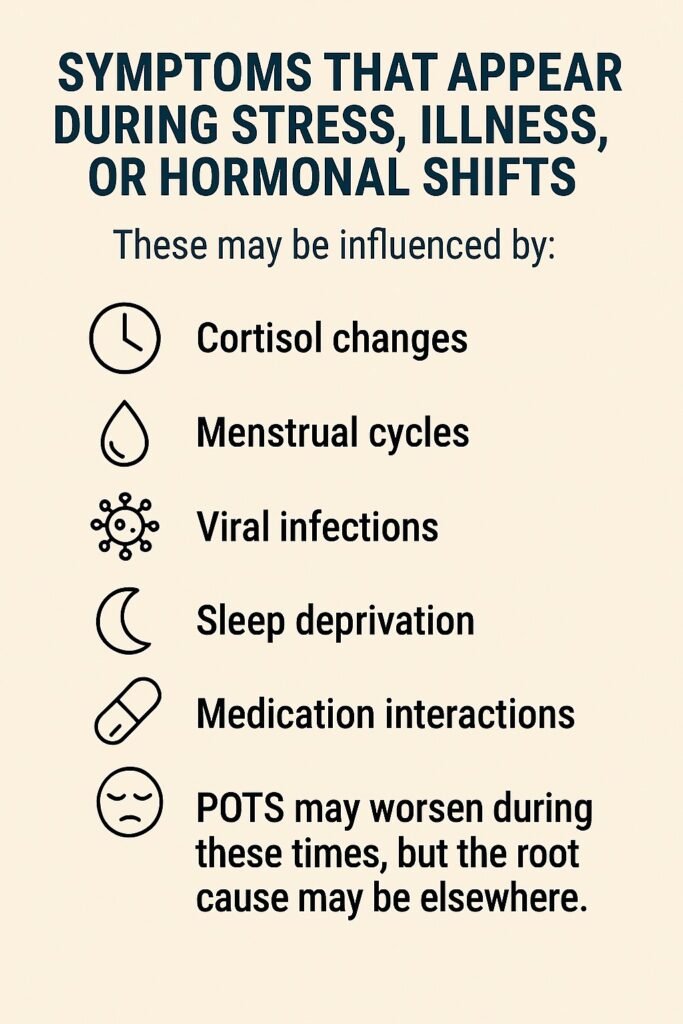
Symptoms That Appear During Stress, Illness, or Hormonal Shifts
These may be influenced by:
- Cortisol changes
- Menstrual cycles
- Viral infections
- Sleep deprivation
- Medication interactions
POTS may worsen during these times, but the root cause may be elsewhere.
When to Tell Your Doctor About New Symptoms
It’s common to wonder whether you should report every new symptom—especially when you already have a long list. A helpful approach is to consider:
Tell your doctor when:
- A symptom is new and persistent
- A symptom is severe or worsening
- A symptom doesn’t match your usual POTS pattern
- A symptom affects daily functioning
- You suspect a medication side effect
- You feel something is “off” in a way you can’t explain
You may not need urgent reporting when:
- The symptom is mild and familiar
- It resolves quickly
- It clearly follows a known trigger (heat, dehydration, standing too long)
- It improves with rest or hydration
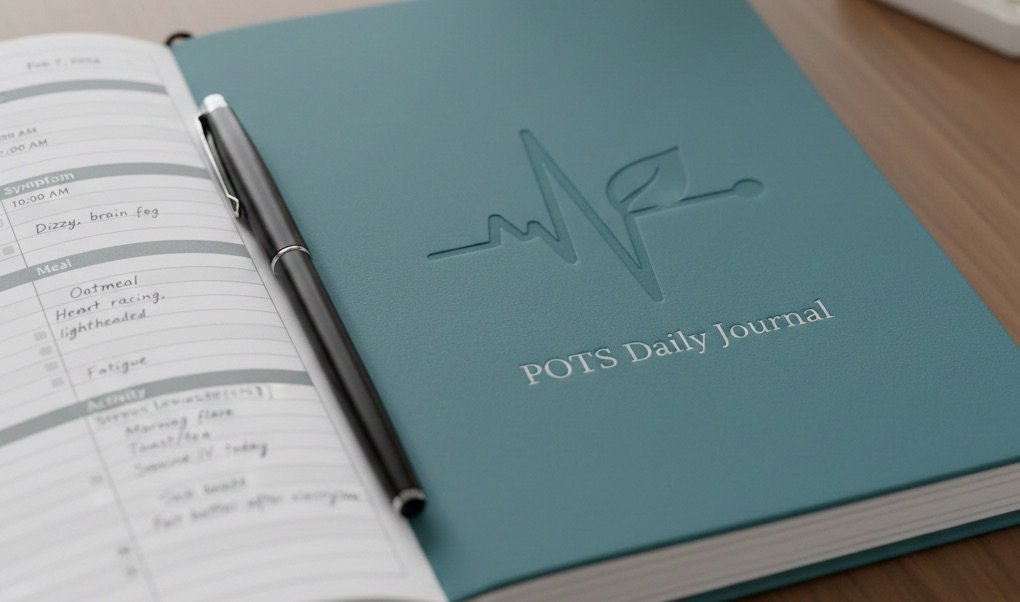
Keeping a symptom journal can help you track patterns without feeling overwhelmed.

Connecting Symptoms to Nutrition, Hydration, and Lifestyle
Nutrition-Related Symptoms
Nutrient deficiencies can mimic or worsen POTS symptoms. For example:
- Low iron or B12 can cause fatigue and dizziness
- Low magnesium can cause muscle cramps or palpitations
- Low sodium intake can worsen orthostatic intolerance
If symptoms appear after dietary changes or inconsistent eating, nutrition may be involved.
Hydration and Electrolytes
Dehydration is one of the fastest ways to trigger POTS symptoms. If symptoms improve after fluids, electrolytes, or salt intake, hydration may be the primary factor.
Exercise and Deconditioning
Exercise intolerance is common in POTS, but:
- Too little movement can worsen symptoms
- Too much or the wrong type of exercise can cause pain, fatigue, or flare-ups
- Incorrect routines may stress joints, muscles, or the autonomic system
If symptoms appear after activity, the type, intensity, or timing of exercise may be the cause—not POTS itself.
The Big Picture: POTS Is One Piece of a Complex Puzzle
Many people with POTS live with multiple overlapping conditions. Instead of trying to assign each symptom to a single cause, it can be more helpful to look at:
- Patterns
- Triggers
- Timing
- Lifestyle factors
- Environmental influences
- Coexisting diagnoses
Your body is giving you information. The goal is not to label every symptom perfectly, but to understand how the pieces fit together so you can manage your health more effectively.

GnarlyTree | DIET AND EATING
Let’s Go Shopping for POTS Friendly Foods
Shopping for POTS friendly foods doesn’t have to feel overwhelming—it can be empowering when you know what to look for and how to build a pantry that works with your body instead of against it....
Frequently Asked Questions
What symptoms are most likely caused by POTS?
Symptoms that worsen with standing, heat, dehydration, or exertion are often related to POTS.
Can POTS cause bone or joint pain?
POTS itself typically does not cause bone pain; joint or bone discomfort often comes from other conditions.
How do I know when to tell my doctor about a new symptom?
If a symptom is new, severe, persistent, or unusual for you, it’s worth mentioning.
Can nutrition affect POTS symptoms?
Yes, hydration, electrolytes, and nutrient levels can significantly influence symptom severity.
How do I know if a symptom is from exercise or from POTS?
If symptoms follow activity, the type or intensity of exercise may be the cause rather than POTS itself.
Do overlapping conditions make POTS symptoms worse?
Yes, conditions like EDS, MCAS, migraines, or autoimmune issues can amplify autonomic symptoms.
Should I track symptoms daily?
Tracking patterns can help you identify triggers and communicate more clearly with your care team.
Can stress make POTS symptoms worse?
Stress affects the autonomic system and can intensify POTS symptoms.
Is it normal for symptoms to change day to day?
Yes, POTS symptoms often fluctuate based on hydration, hormones, sleep, and activity.
Final Thoughts
Sorting out what symptoms come from POTS and what comes from other conditions is not easy—and it’s rarely clear-cut. POTS interacts with nearly every system in the body, and when you add overlapping conditions, the picture becomes even more complex. Instead of trying to label every symptom perfectly, focus on understanding patterns, triggers, and the broader context of your health.
By paying attention to your body, tracking changes, and communicating with your care team
Do you have workplace accommodations for your POTS?