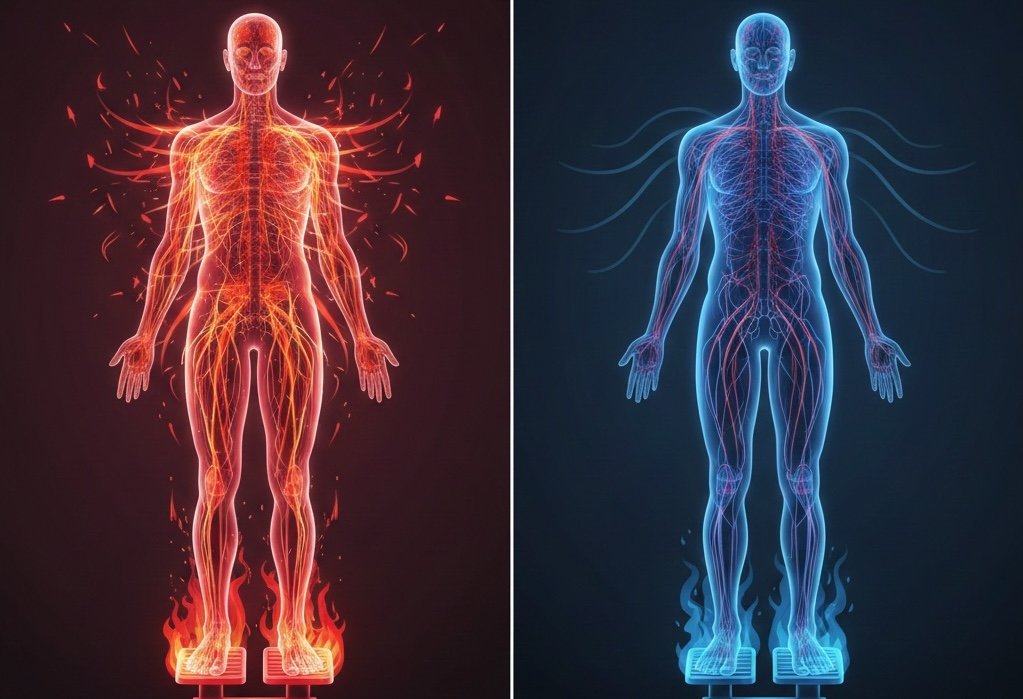
Hyperadrenergic POTS, often abbreviated as HyperPOTS or Adrenergic POTS, is a distinct subtype of Postural Orthostatic Tachycardia Syndrome (POTS). As part of the broader category of dysautonomia, it involves a dysfunction of the autonomic nervous system, leading to an exaggerated sympathetic nervous system response.
This heightened activity results in excessive norepinephrine release, particularly when standing, which can mimic anxiety and complicate diagnosis.
Understanding the Sympathetic Overdrive
Unlike other forms of POTS, Hyperadrenergic POTS is marked by an overactive sympathetic nervous system, causing:
How do you best manage a "POTS bad day"?
- Elevated blood pressure upon standing
- Increased plasma norepinephrine levels
- Symptoms that may resemble anxiety, tremors, and excessive sweating
This subtype requires a nuanced approach to diagnosis and management, as traditional POTS treatments may not fully address the autonomic imbalance.
What Makes Hyperadrenergic POTS Unique?
Hyperadrenergic POTS differs from other subtypes due to its distinct physiological mechanisms. While most POTS cases involve low blood volume or neuropathic dysfunction, HyperPOTS is characterized by excessive sympathetic activation.
Key Differentiators
- Blood Pressure Response: Unlike other POTS subtypes, individuals with HyperPOTS often experience a rise in systolic blood pressure upon standing.
- Norepinephrine Levels: Plasma norepinephrine levels exceed 600 pg/mL, contributing to tachycardia and heightened autonomic responses.
- Comorbidities: Many individuals with HyperPOTS also exhibit signs of mast cell activation syndrome (MCAS), which can exacerbate symptoms An overview of a POTS subtype.
Understanding these unique features is essential for tailoring effective treatment strategies, which often focus on sympathetic modulation rather than traditional volume expansion approaches.
Key Symptoms of Hyperadrenergic POTS
Hyperadrenergic POTS presents a distinct symptom profile due to excessive sympathetic nervous system activation. These symptoms often fluctuate in severity and may be influenced by external factors such as stress, heat, dehydration, or meal timing.
Cardiovascular Symptoms
- Rapid heart rate upon standing (tachycardia), often exceeding 120 BPM
- High blood pressure while upright, unlike other POTS subtypes
- Elevated plasma norepinephrine levels (above 600 pg/mL), contributing to autonomic instability
- Palpitations, often described as a racing or pounding heartbeat
Neurological & Autonomic Symptoms
- Excessive sweating, particularly in response to minor exertion or stress
- Anxiety or panic attack-like episodes, triggered by sympathetic overdrive
- Tremors, sometimes mistaken for essential tremor or anxiety-related shaking
- Insomnia, due to heightened norepinephrine levels interfering with sleep regulation
Additional Symptoms
- Chest pain or pressure, often unrelated to cardiac disease but linked to autonomic dysfunction
- Lightheadedness or dizziness, particularly upon standing or prolonged upright posture
These symptoms tend to be more pronounced in the morning or after meals, as digestion can further stimulate the autonomic nervous system. External stressors such as heat exposure, dehydration, or emotional distress can exacerbate symptom severity, making symptom management a crucial aspect of daily life.
Causes and Contributing Factors
The underlying causes of hyperadrenergic POTS remain complex, with research pointing to a combination of genetic, autoimmune, and environmental influences. Unlike other POTS subtypes, HyperPOTS is often linked to sympathetic nervous system dysregulation, leading to excessive norepinephrine release.
Genetic and Autoimmune Links
- Autoimmune diseases such as Sjögren’s syndrome and lupus may contribute to autonomic dysfunction.
- Genetic predisposition plays a role, with some individuals exhibiting mutations affecting norepinephrine transport.
- Mast Cell Activation Syndrome (MCAS) is frequently associated with HyperPOTS, as mast cell dysfunction can trigger sympathetic overactivation.
Environmental and Infectious Triggers
- Chronic infections, including Epstein-Barr virus, have been implicated in autonomic instability.
- Hormonal imbalances, particularly those affecting adrenal function, may exacerbate symptoms.
- Post-viral onset: Many cases develop after a viral illness, injury, or major surgery, suggesting a link between immune system activation and autonomic dysfunction.
These contributing factors highlight the multifaceted nature of hyperadrenergic POTS, requiring a personalized approach to diagnosis and management.
Diagnosing Hyperadrenergic POTS
Accurate diagnosis is essential, as Hyperadrenergic POTS symptoms often mimic anxiety disorders or cardiovascular conditions. A structured diagnostic approach helps differentiate this subtype from other forms of dysautonomia.
Clinical History and Physical Exam
A thorough symptom review is the first step in diagnosis, focusing on:
- Onset and severity of symptoms
- Triggers such as stress, heat, or dehydration
- Family or personal history of dysautonomia or autoimmune conditions
A physical exam may reveal tachycardia, tremors, or excessive sweating, which are hallmarks of sympathetic overactivation.
Tilt Table Test
This test evaluates changes in heart rate and blood pressure in response to positional changes. In hyperadrenergic POTS, a sustained increase in heart rate and often blood pressure is observed.

Plasma Norepinephrine Levels
Blood samples are taken while the patient is standing to measure norepinephrine. Levels above 600 pg/mL are indicative of hyperadrenergic activity.
Additional Tests
- 24-hour blood pressure and heart rate monitoring
- Urine catecholamines
- Autonomic reflex screening
Managing Hyperadrenergic POTS
Treatment for hyperadrenergic POTS is often multifaceted, involving lifestyle changes, medications, and supportive therapies.
Lifestyle Modifications

- Increase salt and fluid intake: Typically 2-3 liters of water and 3,000–5,000 mg of sodium daily
- Regular recumbent exercise: Activities like rowing, swimming, and recumbent cycling help improve cardiovascular tone without triggering symptoms
- Avoid triggers: Heat, alcohol, high carbohydrate meals, and prolonged standing
- Compression garments: Waist-high compression socks or abdominal binders support venous return
Medications
Medication plans should be personalized and may include:
- Beta blockers: Reduce heart rate and lower sympathetic activity
- Clonidine or Methyldopa: Decrease norepinephrine production
- Ivabradine: Lowers heart rate without affecting blood pressure
- Antihistamines: Useful if MCAS is a comorbidity

Nutritional Support and Supplements
Anti-inflammatory diets rich in omega-3 fatty acids, antioxidants, and complex carbohydrates can help stabilize symptoms. Supplements like magnesium, B-vitamins, and CoQ10 are also commonly recommended.

Living with Hyperadrenergic POTS and Dysautonomia
Hyperadrenergic POTS can be life-altering, but with proper care and support, many individuals find ways to effectively manage their symptoms. Adapting daily routines and implementing targeted strategies can significantly improve quality of life.
Mental Health Considerations
Because Hyperadrenergic POTS can mimic anxiety disorders, addressing mental health is a crucial part of symptom management. Supportive interventions include:
- Counseling to help navigate the emotional impact of chronic illness
- Cognitive Behavioral Therapy (CBT) to manage anxiety-like symptoms
- Mindfulness practices, such as meditation and breathing exercises, to regulate autonomic responses
Many individuals benefit from integrating mental health care into their overall treatment plan, ensuring a holistic approach to managing Hyperadrenergic POTS.
Community and Support Resources
Navigating Hyperadrenergic POTS can be challenging, but connecting with support organizations and online communities can provide education, advocacy, and emotional support.
Key Organizations
Standing Up to POTS – Focuses on research, advocacy, and patient support, offering resources for individuals with POTS.
Awareness for POTSies – Shares insights on different POTS types and promotes community engagement.
Dysautonomia Information Network (DINET) – Provides detailed information on POTS subtypes, including Hyperadrenergic POTS.
Online Support Groups
Many individuals find peer support invaluable. Engaging in forums, social media groups, and virtual meetups can help with:
- Sharing experiences and symptom management strategies
- Finding medical professionals familiar with POTS
- Accessing new research and treatment updates
Share Your Story Here at GnarlyTree


GnarlyTree | SUPPLEMENTS
Address Nutritional Deficiencies with POTS | Identifying and Filling the Gaps
While treatment often includes medication and lifestyle changes, addressing nutritional deficiencies with POTS plays a crucial role in symptom management. For individuals with POTS, optimizing diet nutrition is not just about eating well—it’s a foundational...
Frequently Asked Questions
Is Hyperadrenergic POTS the most severe form?
Not necessarily. While its symptoms can be more distressing due to sympathetic nervous system overactivation, severity varies among individuals. Some experience mild symptoms, while others face significant daily challenges.
Can it be cured?
There is currently no cure, but symptoms can often be managed effectively with a comprehensive treatment plan. Strategies may include:
- Medications to regulate autonomic function
- Lifestyle modifications such as hydration, dietary adjustments, and stress management
- Physical therapy to improve circulation and autonomic stability
What is the prognosis?
Prognosis varies widely. Some individuals experience gradual improvement, while others manage chronic symptoms long-term. Factors influencing prognosis include:
- Underlying conditions such as autoimmune disorders or mast cell activation syndrome
- Effectiveness of symptom management strategies
- Individual response to treatment and lifestyle adjustments
Conclusion
Hyperadrenergic POTS is a complex but manageable form of dysautonomia, distinguished by sympathetic nervous system overactivity. This heightened autonomic response leads to a unique symptom profile, requiring tailored diagnostic and treatment approaches.
Key Takeaways
- Sympathetic overactivation drives symptoms such as tachycardia, elevated blood pressure, and anxiety-like episodes.
- Understanding POTS subtypes is essential for effective care, as treatment strategies differ based on the underlying autonomic dysfunction.
- Early diagnosis and targeted management can significantly improve quality of life, helping individuals navigate daily challenges.
If you or someone you know is experiencing unexplained tachycardia, high blood pressure when upright, and symptoms resembling anxiety, consulting a healthcare provider familiar with POTS and dysautonomia is crucial for proper evaluation and care.

What exercise equipment do you find most helpful for POTS?